Ms Sarah Fitt was appointed Chief Executive of PHARMAC in January 2018, having been PHARMAC's Director of Operations since 2013. As Director of Operations, Ms Fitt led the pharmaceutical funding, devices funding, procurement and contracts and health economics teams.
Ms Fitt graduated in pharmacy from the University of London and worked as a clinical pharmacist in NHS specializing in HIV, intensive care and hepatology. She moved to New Zealand to work at the NZ Liver Transplant Unit and was appointed Chief Pharmacist at Auckland DHB in 2000 where she led a large comprehensive pharmacy service before her appointment to the senior leadership team at PHARMAC in 2013.
Presentation Synopsis
PHARMAC's Influence on New Zealand Healthcare
PHARMAC was established in 1993 and is the New Zealand government agency that decides what medicines are publicly funded in hospitals and the community.
The PHARMAC management model achieves the best possible health outcomes from fixed funding, including making evidence-based decisions informed by expert advice, applying commercial strategies to achieve competitive pricing, comparing new products and prioritizing their funding based on options which will deliver the best health outcomes.
PHARMAC is unique among international central funders - combining a technology assessment agency with commercial negotiations and budget management.
PHARMAC's Work in Managing Medical Devices
In 2012, the New Zealand Government decided that the PHARMAC management model should be applied to the management of hospital medical devices in the 20 District Health Boards (DHBs) in New Zealand.
The PHARMAC management model achieves the best possible health outcomes from fixed funding, including making evidence-based decisions informed by expert clinical advice, applying commercial strategies to achieve competitive pricing and comparing new products and prioritising their funding based on which options will deliver the best health outcomes.
Work completed so far includes gathering feedback through extensive consultation to develop a proposed approach for medical devices management; building a list of medical devices in use through negotiating national contracts and then developing an understanding of the listed products.
Consultation is currently underway to embark on the next phase where PHARMAC will be responsible for deciding which devices are funded.
The new approach is about:
• supporting more consistent access to medical devices across New Zealand
• aid DHBs manage spending in a sustainable way
• free up funding which may be used for new technology or other health initiatives
• ensure there is a high level of transparency around funding decisions
Adjunct Associate Prof Seow Wan Tew is Senior Consultant in the Department of Neurosurgery at the National Neuroscience Institute (NNI) and KK Women’s & Children’s Hospital (KKH). He was Director of Quality in NNI from 2009 till 2015. He was NNI’s Institution Risk Officer from 2010 till 2018 and is currently its Chief Risk Officer.
Prof Seow has strong interest in medico-legal matters and is actively involved in risk management education. He is a facilitator for MPS’ risk management education programs and a teaching faculty of Singapore Medical Association’s Centre for Medical Ethics & Professionalism. He is a member of the Academy of Medicine’s Medical Experts Committee. He helps review NNI’s potential medico-legal cases and is an Associate Mediator with the Singapore Mediation Centre.
Presentation Synopsis
Medico-legal Risk Management – Where are We Heading?
Patients can become dissatisfied with the healthcare we provide and they do express their unhappiness in many different ways – complaints to the MOH, MPs, newspapers, social media, SMC or through litigation. Medico-legal suits against hospitals and doctors for negligence are not common in Singapore but the recent negligence cases - Noor Azlin v CGH and the Hii Chii Kok case - have brought this area of risk management to the forefront. Losing a negligence suit is costly, both financially and from loss of reputation. They take years to settle and the medical staff involved can end up psychologically stressed and burnt-out. They also highlighted the importance of having proper documentation of patients’ informed consent; especially now that electronic medical records are the norm.
The literature suggests that most medico-legal suits are the result of unmet patient expectations and poor doctor-patient communications. It also shows that healthcare organisations that manage their medico-legal risks proactively are able to successfully reduce their number of litigation cases.
Management of medico-legal risks requires a two-pronged approach – prevention and containment, and both have to be done simultaneously. However, in Singapore, these approaches tend to be reactive. More should also be done to help patients resolve their complaints early through open disclosure and clinical incident management and working collaboratively with them to achieve the best outcome.
Dr Siaw Tung Yeng is a Senior Consultant Family Physician with more than 30 years of experience in healthcare and medical informatics. He is an ASEAN scholar and graduated with a Masters in Family Medicine, having spent part of his training in Adelaide (Australia) and the United Kingdom.
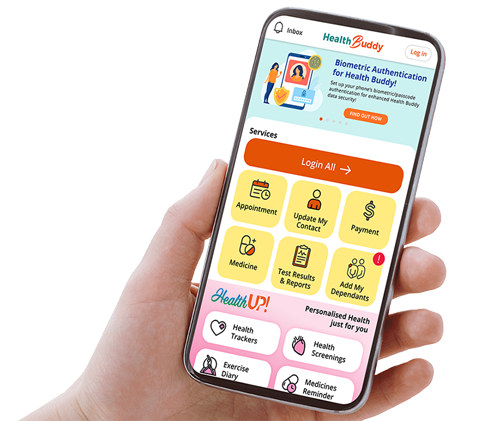
Dr Siaw is the founder and CEO of MaNaDr, which allows patients to book appointments on-line with doctors and tele-consult with them 24/7. He is also a director of UVH, a company which runs a chain of GP clinics and the Medical Director of GLOCO which provides a wide range of innovative IT healthcare solutions throughout ASEAN.
Dr Siaw also sits on various MOH task forces and advisory committees and is actively involved in the strategic planning of medical informatics programmes. He is also a member of the National Telemedicine Advisory Committee (NTAC) and sits in the Singapore Medical Council (SMC) Disciplinary Tribunal currently.
In his presentation, Dr Siaw will be sharing MaNaDr’s digital journey - the opportunities that it offers patients to enjoy affordable, quality healthcare as and when they need it, as well as the challenges and risks faced.
Presentation Synopsis
MaNaDr – A Trusted, Connected, Dynamic and Transformative Healthcare Platform: Challenges & Opportunities in Clinical Application
Mobile technology is so pervasive today that it is inevitable that the mobile platform will become more relevant in the delivery of good, affordable and accessible healthcare. MaNaDr’s digital journey, especially the opportunities, obstacles faced and the support it garnered will be discussed in this talk. The talk will focus on how MaNaDr leverages on the power of AI and smart application of data to deliver transformative patient-centric care services. The challenges/risks ahead and how MaNaDr intends to scale and mitigate them will be also shared. Finally, the talk will explore whether MaNaDr will be the healthcare OS/platform that connects the patient to trusted care providers from cradle to grave, and the solution to “humanize” IT in healthcare delivery.
Dr Stephen Klasko is a transformative leader and advocate for a revolution in health care and higher education.
As President and CEO of Philadelphia-based Thomas Jefferson University and Jefferson Health since 2013, he leads the nation’s fastest growing academic health institution based on his vision of re-imagining the future. Jefferson Health grew from 3 hospitals in 2013 to 14 hospitals in 2018. His 2017 merger of Thomas Jefferson University with Philadelphia University created a professional university with top-20 programmes in fashion, design, health, and the first design-thinking curriculum in a medical school.
His track record earned him a place as #2 “Most Influential” individuals in healthcare by Modern Healthcare, as #21 in Fast Company’s 100 Most Creative People in Business 2018 and Philadelphia Entrepreneur of the Year 2018.
He was responsible for naming two of the nation's medical schools through transformational gifts: The Morsani College of Medicine at the University of South Florida, where he was dean and CEO of USF Health from 2004-2013; and the Sidney Kimmel Medical College at Thomas Jefferson University.
Presentation Synopsis
Becoming A 200-year-old Start-Up
Academic health centres play a critical role in their communities - in advancing science, education, and direct medical care. However, legacy infrastructure, culture and practice threaten the future of some of our most prestigious institutions, and challenge their roles as "anchors" in their cities. This talk will examine how a "no limits" approach can transform a distinguished history.
Is There an Avatar in the House? Healthcare in the Age of AI
In an age of profound change, physicians increasingly need the tools of creativity, communication and optimism. Starting with medical education, we need a revolution in how doctors are selected and taught to practice with AI, to ensure that doctors are the humans in the room, even if that room is virtual.